Children born with congenital heart defects (CHDs) often face significant challenges, but their resilience and spirit inspire everyone around them. These are structural abnormalities of the heart that are present from birth and can vary widely in severity—from minor issues that require minimal intervention to complex conditions that pose significant health challenges. Gaining a clear understanding of these conditions is crucial for parents, caregivers, and anyone interested in pediatric health, as early diagnosis and appropriate management can truly transform a child's future and improve their quality of life.
What Are Congenital Heart Defects?
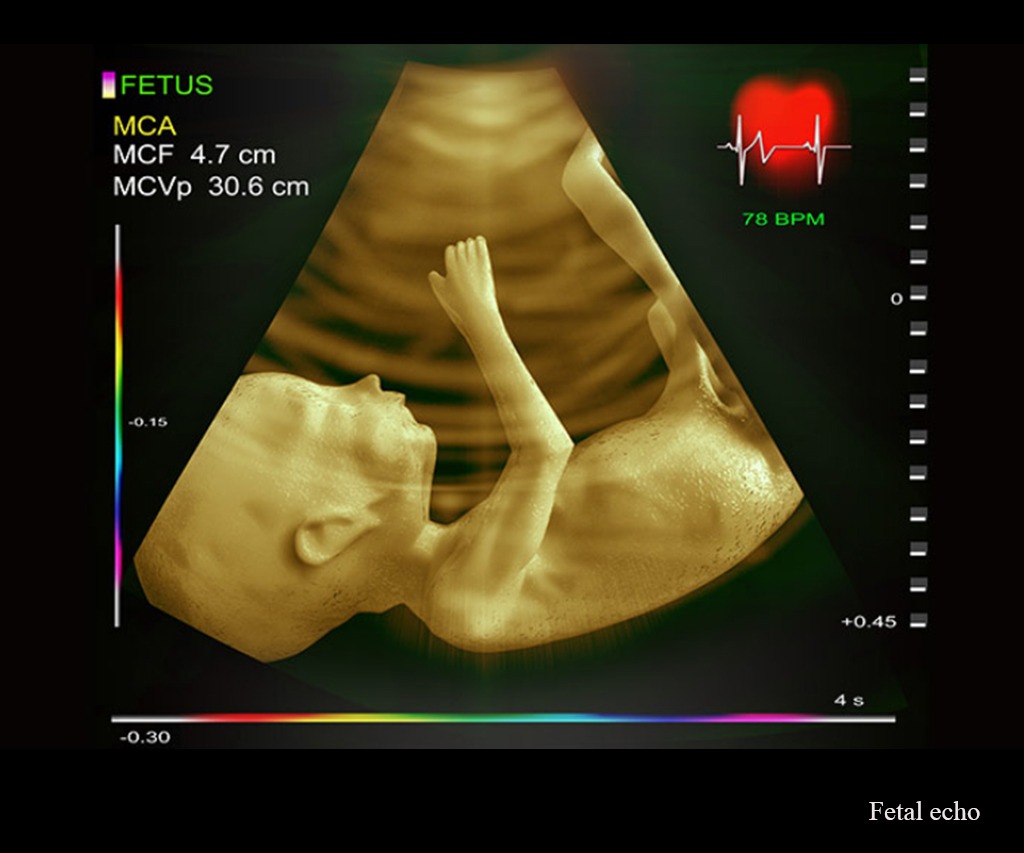
Congenital heart defects are abnormalities in the structure of a child's heart that develop during fetal life. They can involve the walls of the heart, the valves, or the large blood vessels that carry blood to and from the heart. While some defects are mild and may not cause symptoms or require intervention, others can be complex and demand lifelong management. My role as a specialist involves diagnosing these conditions early and guiding treatment to ensure the child leads a healthy, active life.
Types of Congenital Heart Defects
There are different types of CHDs, each with its own set of features:
Septal Defects:
These include atrial septal defects (ASD) and ventricular septal defects (VSD). Think of these as small openings or holes in the wall separating the heart's upper chambers (atria) or lower chambers (ventricles). While some may close on their own, others require intervention to prevent complications like congestive heart failure.
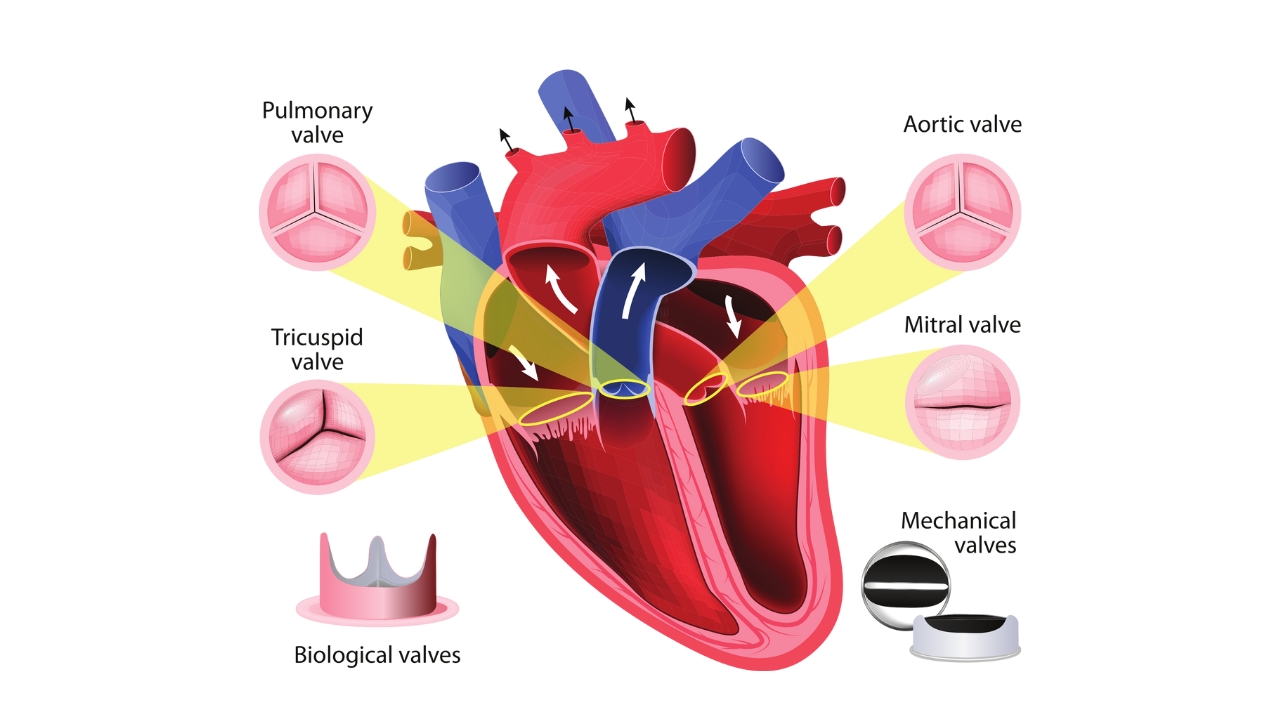
Heart Valve Defects:
Valves regulate blood flow within the heart. When these valves are narrowed (stenosis) or leaky (regurgitation), the heart must work harder, which can cause symptoms such as fatigue, coughing, or swelling. Depending on the severity, treatment might involve balloon dilation or surgical repair.
Defects in Large Blood Vessels:
One common example is coarctation of the aorta—a narrowing of the main artery supplying blood to the body. This can cause high blood pressure and decreased blood flow if left untreated.
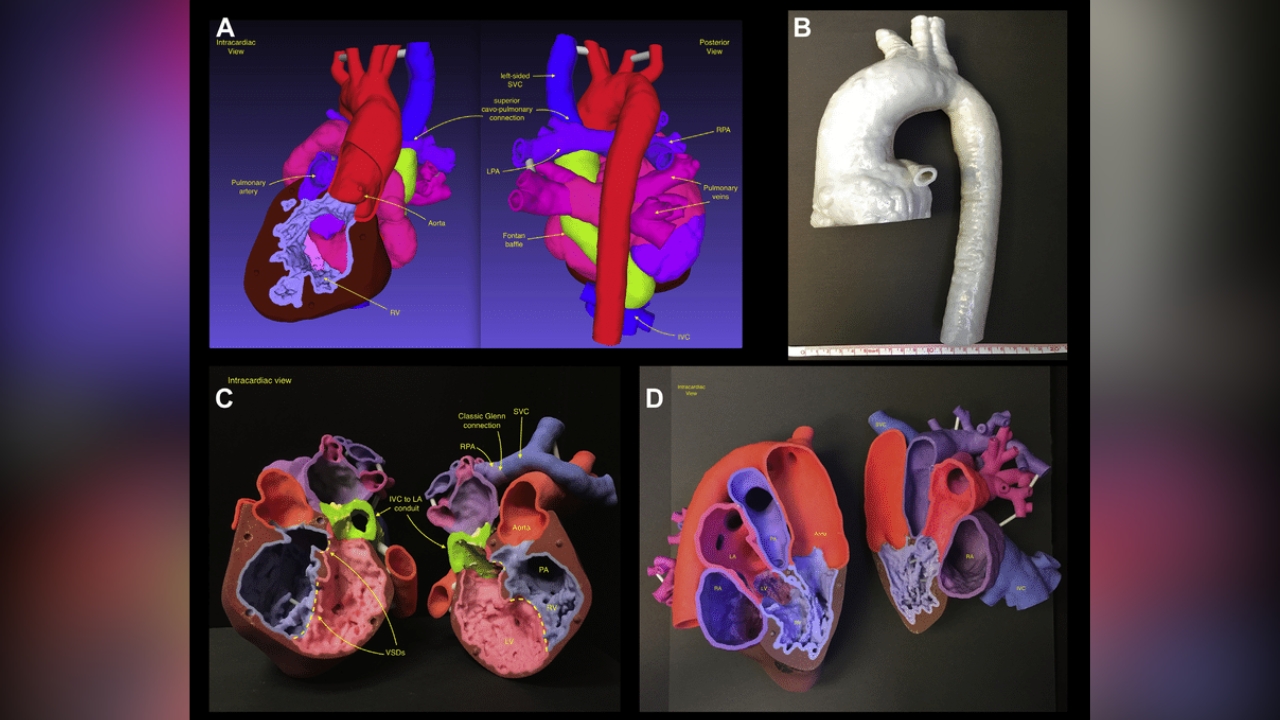
Complex Defects:
Some children have multiple structural problems or missing parts of the heart, such as in Tetralogy of Fallot—a combination of four defects that can cause oxygen-poor blood to circulate throughout the body. These situations require comprehensive management, often from birth.
Causes, Symptoms, and Treatments
Causes:
The exact causes of congenital heart defects are often unknown. Sometimes, genetic factors, maternal health issues (such as diabetes or infections during pregnancy), environmental exposures, or certain medications during pregnancy can contribute. Usually, it’s a combination of factors, and in many cases, the exact cause remains elusive.
Symptoms:
Symptoms can vary based on the defect. Common signs include rapid breathing, fatigue, poor feeding, bluish tint to the skin (cyanosis), and failure to thrive. Sometimes, the diagnosis is suggested by a heart murmur—an abnormal sound heard during routine examinations.
Treatments:
Management depends on the specific defect and its severity. Minor defects might close spontaneously or may only need monitoring. Other cases require catheter-based interventions like device closures or open-heart surgeries. Timely diagnosis through echocardiography is critical—early treatment prevents complications, promotes normal growth, and helps children lead active lives.
Patient Story: A Heartfelt Journey
I remember Rohan, a curious toddler who was slow to gain weight and tired during play. His parents were concerned, and a detailed echocardiogram revealed a VSD, a small hole in his heart. Because we detected it early, Rohan underwent a minimally invasive device closure. Within days, he was back to his lively self. Today, he dashes around with no symptoms, thanks to timely intervention.
Final Thoughts
Understanding congenital heart defects is vital for ensuring children receive the care they need. With advancements in diagnostic techniques and surgical procedures, many kids with CHDs live full, active lives. If your child shows signs of fatigue, difficulty breathing, or other health concerns, consulting a pediatric cardiologist can make all the difference. Early detection and management are the keys to a healthier, happier future.
Add a Comment