It’s completely understandable to be anxious about a child undergoing neurosurgery. However, pediatric neurosurgery today is highly advanced and very safe in expert hands. Children’s bodies (and brains) actually heal faster and better than adults in many cases. Dr. Murali and pediatric neurosurgeons like him have training and experience specifically in the delicate care that children require. Surgeries on babies – even newborns – have been done successfully when needed. In fact, brain surgeries for conditions in infants (even just-born babies) can be performed with utmost safety. We use specialized pediatric anesthesia teams (to ensure the child is pain-free and stable during surgery) and tools that are appropriate for smaller bodies. Advances in technology, such as neuronavigation (like a GPS for the surgeon) and microscopes, apply to children’s surgeries as well, making them precise. One important aspect is that kids are resilient – a child’s brain can adapt and bounce back amazingly well after, say, removal of a tumor or correction of a defect, especially if the surgery is done early enough to prevent damage. We also pay extra attention to the child’s comfort and developmental needs: for example, we involve pediatric intensivists, neurologists, and rehab specialists in the care. The outcomes in pediatric neurosurgery are often excellent. The track record for pediatric neurosurgical procedures is very reassuring. Our team will take every precaution and treat your child as if they were our own. Many parents find that after the successful surgery, their biggest reward is seeing their child return to smiling, playing, and developing on track – and that is our biggest reward too. In summary, yes, neurosurgery in children is safe and often life-saving or life-changing, and it’s conducted with the highest level of care and compassion for our little patients

Dr. Murali Mohan S
Precision in Surgery. Passion in Innovation. Purpose in Care.
MBBS, DNB (Neurosurgery)
23+ Years in Neurosurgery
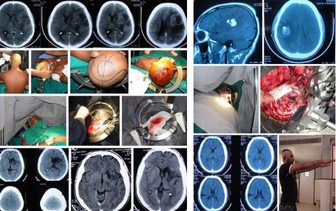
30000+ Patients | 8000+ Surgeries


About Dr. Murali Mohan S
Dr. Murali Mohan S is a leading Neurosurgeon, Healthcare Entrepreneur, Innovator, and an influential thought leader advancing brain and spine care. With over 8,000 brain and spine surgeries performed. He has earned recognition for his surgical expertise in Complex Neurosurgical Procedures. He holds a patent for an indigenous stereotactic frame, founded Dr. Klinisch Research Pvt Ltd. for clinical research, and created LinQMD, an AI-powered platform for doctors’ digital presence. He currently serves as Lead Consultant, Neurosciences at Sparsh Hospital, Hennur. Beyond the operating room, Dr. Murali is a TEDx speaker, blogger, biker, and astronomy enthusiast—leading with ‘clarity, curiosity, and vision across healthcare innovation, research, and communication.
As Lead Consultant, Neurosciences at Sparsh Hospital, Hennur—a Centre of Excellence for Neurosciences—Dr. Murali Mohan S delivers advanced, patient-focused care across brain and spine surgery. His expertise spans brain tumors, skull base surgery, craniovertebral junction stabilization, spinal surgeries including deformities and complex spine reconstructions. With over 8,000 surgeries, he blends microsurgical precision, minimally invasive techniques, and compassionate care to optimize neurological outcomes. Dr. Murali also consults at Synapse Clinics in Jayanagar and Yelahanka, extending expert access beyond hospital walls. Patients trust him for his surgical skill, clear communication, and unwavering commitment to their recovery journey.

Dr. Murali Mohan S's Areas of expertise
Dr. Murali Mohan S offers comprehensive neurosurgical expertise across brain and spine conditions, combining advanced surgical techniques with patient centered care. His work spans pediatric, adult, and geriatric neurosurgery, with a special focus on complex, minimally invasive, and reconstructive procedures. With over 8,000 surgeries, Dr. Murali is trusted for delivering precision outcomes across a wide spectrum of neurological conditions.
Brain Tumor Management: Surgical and non-surgical approaches to diagnose and treat benign and malignant brain tumors to improve outcomes and quality of life.
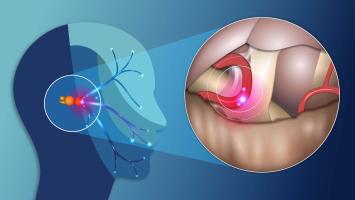
Deep Brain Stimulation (DBS) for Parkinson’s Disease: A minimally invasive procedure that implants electrodes to help regulate abnormal brain activity, improving motor symptoms.
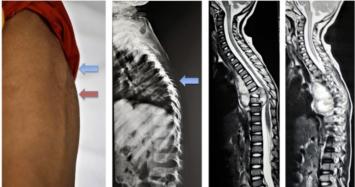
Spinal Deformities Correction (Scoliosis, Kyphosis, Degenerative Disorders): Surgical treatment to straighten or stabilize abnormal spinal curvatures and degenerative changes for pain relief and function.
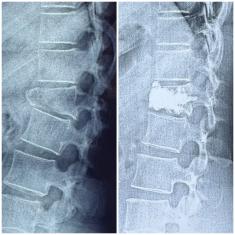
Complex Spine Surgeries (Cervical and Lumbar Spondylosis, Total Disc Replacement): Advanced procedures to treat degenerative disc disease and spinal instability, restoring movement and reducing pain.
Pediatric Brain and Spine Surgeries: Specialized surgeries for neurological conditions in children, including tumors, congenital anomalies, and traumatic injuries.
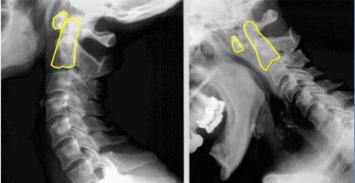
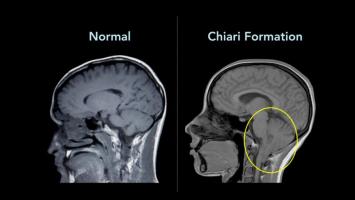
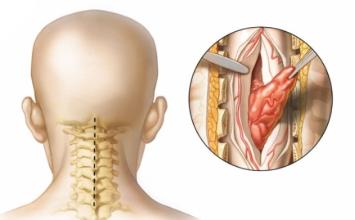
Craniovertebral (CV) Junction Disorders: Surgical management of disorders affecting the skull-base and upper cervical spine to prevent neurological damage.
Back Pain and Disc Disorder Treatment: Medical and surgical options to relieve pain caused by disc herniation, degeneration, or spinal instability.
Brain and Spine Infection Management: Diagnosis and treatment of infectious conditions like abscesses or meningitis affecting the brain and spinal cord.
Spasticity and Epilepsy Treatment: Managing muscle stiffness and seizures through medication, surgical, or neuromodulation techniques.
Minimally Invasive Neurosurgical Techniques: Use of small incisions and advanced technology to reduce surgical trauma and enhance recovery.
Head Injury Care: Emergency assessment and surgical intervention to manage traumatic brain injuries and intracranial hematomas.
Osteoporotic Spine Fractures Management: Vertebral augmentation procedures like kyphoplasty and vertebroplasty to stabilize fractures and reduce pain.
Geriatric Spine Surgery: Customized surgical care tailored for older adults, focusing on safety, rehabilitation, and preserving independence.
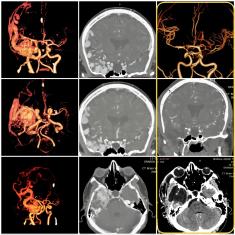
Aneurysm and AVM (Vascular Neurosurgery): Microsurgical techniques to clip aneurysms and remove arteriovenous malformations, preventing hemorrhage.
Stroke Prevention Surgery: Procedures like carotid endarterectomy to reduce the risk of stroke caused by narrowed arteries.
Emergency Neurosurgery: Immediate surgical interventions for life-threatening conditions like traumatic injuries, bleeding, or strokes.
Focused Neuro ICU Care: Intensive management of critically ill neurological patients to optimize recovery and prevent complications.
Neurorehabilitation: Long-term therapy programs aimed at restoring function and improving quality of life after neurological injuries.
Dr. Murali Mohan S has contributed extensively to neurosurgical research, clinical publications, and academic discourse, with award-winning papers, peer-reviewed journal articles, and textbook chapters. His work reflects a deep commitment to advancing neurosurgical knowledge and practice.
Award Paper Presentations
Suboccipital Segment of Vertebral Artery – A Cadaveric Study Neurological Society of India Conference, Madurai (Dec 2006)
Rhino-cerebral Fungal Granuloma, Skull Base Society of India & WFNS Conference, New Delhi (Oct 2007)
Surgery of Craniovertebral Junction, Skull Base Society of India & WFNS Conference, Jaipur (Oct 2016)
Journal Publications
Suprasellar Germ Cell Tumor… J Pediatr Endocrinol Metab, 2003
Intracranial Epithelioid Hemangioendothelioma… Childs Nerv Syst, 2008
Pediatric Medulloblastoma: Review of 67 Cases… Asian J Neurosurg, 2008
Suboccipital Segment of Vertebral Artery… Neurol India, 2009
Invasive Rhino-Cerebral Fungal Granuloma… Neurol India, 2010
Morphometric Analysis of Thoracic Pedicle… Neurol India, 2010
Intraoperative Angiography in Cerebral Aneurysm Surgery… Neurol India, 2010
"A Useful Noise in the Operating Room"… J Cerebrovasc Sci, 2015
“Retraction-less Aneurysm Surgery”… J Cerebrovasc Sci, 2015
Pial AV Fistula Presenting as Lobar Hemorrhage… J Cerebrovasc Sci, 2015
Intraventricular Gliosarcomas… World Neurosurg, 2016
Textbook Chapters
Surgical Anatomy of Posterior Third Ventricle – Textbook of Operative Neurosurgery
Empty Sella Syndrome – Ramamurthi & Tandon Textbook of Neurosurgery
Acoustic Neurofibroma – Ramamurthi & Tandon Textbook of Neurosurgery
Stereotaxy for Brain Tumors – Ramamurthi & Tandon Textbook of Neurosurgery
Diencephalic Syndrome – Ramamurthi & Tandon Textbook of Neurosurgery
Bacterial Infections of the Spine – Text of Neurosurgery
Tuberculosis of CNS – Text of Neurosurgery
Information Systems for Knowledge Management… – Knowledge Organisation
Anatomy of the Sellar and Suprasellar Region – Textbook of Endocrinology
Pituitary Adenoma; Growth Hormone Secreting Pituitary Adenomas; Corticotroph Adenomas; Prolactinoma; Other Pituitary Adenomas – Textbook of Endocrinology
Endoscopic Lumbar Discectomy; Endoscopic Surgery for Pituitary Tumors – Clinical Neuroendoscopy
Professional Memberships
Neurological Society of India
Skull Base Surgery Society of India
Association of Spinal Surgeons of India
Bangalore Neurological Society
Indian Federation of Neuro-endoscopy
Indian Association of Pediatric Neurosurgery
- MBBS - 2001, Rajiv Gandhi University of Health Sciences, Karnataka.
- DNB Neurosurgery - 2008, National Board of Examinations, New Delhi.
Dr. Murali Mohan S is a senior consultant Neurosurgeon from Bengaluru. Having completed his graduation from MS Ramaiah Medical College, RGUHS, He received his Neurosurgical training under Prof B Ramamurthi DSc (the father figure of Indian Neurosurgery) and the team of Senior & accomplished Neurosurgeons: Dr Ravi Ramamurthi, Dr MC Vasudevan, Dr Krish Sridhar and Dr Anil Pande, at the Post graduate Institute of Neurological Surgery, ALNC, VHS Hospital, Chennai.
Dr Murali gained further expertise in this field by working with renowned Neurosurgeons - Prof RM Varma, Dr AS Hegde, Dr Venkataramana NK, Dr Balaji Pai, Dr Ravi Gopal Varma and Doyen of Spine Surgery - Dr Thierry Marnay (Montpellier, France).
Book Appointment
Major Akshay Girish Kumar Rd, Yelahanka Satellite Town, Yelahanka, Bengaluru, Karnataka 560064
- Monday
- 03:00 PM to 04:30 PM
Phone: +91 80501 57007 | +91 99007 01080
Email: [email protected]
771, 10th Main Road, 34th Cross Rd, 4th Block, Jayanagar, Bengaluru, Karnataka 560011
- Tuesday
- 03:30 PM to 04:30 PM
Phone: +91 99027 97944 | +91 99007 01080
Email: [email protected]
HBR Layout, Hennur Road, Bengaluru - 560 043
- Monday - Friday
- 10:00 AM to 01:00 PM
Phone: +91 9686911560 | +91 990701080
Email: [email protected]
Patient Reviews
Dr.Murali Mohan S
AI Summary
5 reviews • 5★
Deepthi PR
3 months ago
Nandini Kutty
2 months ago
Subramanian Sundararajan
2 months ago
Anudeepikas
3 months ago
ashwini kavtekar
a month ago
Conditions and Treatments
Dr. Murali Mohan S's Expert Tips & Health Insights
Articles by Dr. Murali Mohan S

Moments: The reflection of life as it unfolds
While - the trilogy: The Journey · Moments · Presence

7 Point Spine Starter Guide: Simple steps to nurture your Spine
Invest in Your Spine: World Spine Day 2025

Built to Solve: Why Innovation in India Needs a New Lens

Raising Awareness About Scoliosis

The Third Eye

Life as a Neurosurgeon

Food Consciousness

Journey Of Life

The Aging Paradox
Podcasts by Dr. Murali Mohan S
Gallery of Dr. Murali Mohan S
Frequently Asked Questions
Frequently Asked Questions
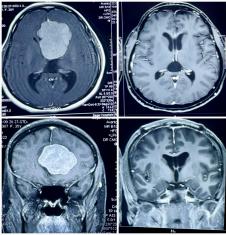
Unfortunately, children can develop tumors in the brain or spine. In fact, brain tumors are the second most common type of childhood cancer (after leukemia). The types of tumors children get are often different from adult tumors – for example, juveniles might develop medulloblastomas, pilocytic astrocytomas, ependymomas, or others. The good news is that many pediatric brain tumors are quite treatable. Treatment usually involves surgery (to remove as much of the tumor as safely possible) and may be followed by chemotherapy or radiation therapy, depending on the tumor type. Children actually often handle chemotherapy better than adults, and special protocols exist to treat pediatric tumors. The prognosis or outlook varies by tumor type and location, but it has improved dramatically over the past few decades. While the word “tumor” is scary, families can take heart that there is a lot of hope – most pediatric tumors can be treated, and the majority of children survive and even thrive after treatment
Craniosynostosis (sometimes called craniostenosis) is a condition in which one or more of the sutures in a baby’s skull close (fuse) too early. These sutures are like expansion joints that allow the skull (and brain) to grow. When a suture fuses prematurely, it can lead to an abnormally shaped head and, more importantly, can constrain the growing brain. If not corrected, it might cause increased pressure on the brain and potential developmental issues. Early surgery is the treatment for craniosynostosis. The neurosurgeon will open the fused suture and reshape the skull bones. This procedure, done in infancy (usually before 1 year of age, often around 6–9 months old), allows the brain to grow normally and also improves the head’s shape. Cosmetic correction isn’t just about appearance – a more typical skull shape can positively impact the child’s social and psychological development, as the child won’t have to grow up with an unusual head shape. The surgery might sound daunting, but it is generally very successful. Babies’ skulls are soft and heal quickly. After the expansion surgery, the brain has the space it needs, and typically the child’s development proceeds normally. In short, craniosynostosis is a mechanical issue (bones fused too early) that we fix mechanically (by reopening and correcting the bones), and doing so early prevents brain damage and sets the child up for normal growth
Hydrocephalus is often known as “water on the brain.” It’s a condition where the cerebrospinal fluid (CSF) that bathes the brain doesn’t circulate or drain properly, causing an excess of fluid in the brain’s ventricles (hollow spaces). In infants and children, this can make the head enlarge and put pressure on the developing brain, leading to symptoms like a rapidly growing head size, bulging soft spot, seizures, or developmental delays. The good news is that hydrocephalus can be very effectively treated. The most common treatment is placing a VP shunt (ventriculoperitoneal shunt). A shunt is a thin, flexible tube that neurosurgeons implant; it diverts the extra fluid from the brain to another part of the body (usually the abdomen) where it can be absorbed. This relieves the pressure on the brain. Another treatment in some cases (especially older children) is an endoscopic third ventriculostomy (ETV), where using a tiny camera, the surgeon creates a small hole in one of the ventricle walls to bypass the blockage and let fluid flow out normally, sometimes avoiding the need for a shunt. With timely diagnosis and treatment, children with hydrocephalus can lead normal, healthy lives.
Neural tube defects are birth defects of the brain or spine that occur very early in pregnancy (when the neural tube, which forms the spinal cord and brain, doesn’t close properly). One common example is spina bifida (myelomeningocele), where a portion of the spinal cord and nerves develop outside the body, often in a sac on the baby’s back. These conditions can sound scary, but yes, they can be treated. In fact, for spina bifida, surgery is usually done within the first one or two days of a baby’s life to gently place the spinal cord and nerves back inside and close the opening. This prevents infection and further injury to the spinal cord. The early surgery greatly improves outcomes – it protects the nerves from ongoing damage. Some children with spina bifida will have weak leg movement or need assistance devices later, but many go on to live active lives, especially with modern therapies. Neural tube defects like encephalocele (where part of the brain protrudes through a skull opening) are also usually treated surgically early in life. The key point is: with timely neurosurgical intervention and follow-up care, babies born with these conditions can often be saved from severe disability and given a chance at a healthy life.
This is a common fear stemming from the past, but it’s largely outdated now. Decades ago, spine surgeries (for things like disc problems or spine injuries) had more variable outcomes, but technology and surgical skill have advanced leaps and bounds. Today, spine surgeons use tools like operating microscopes, neuronavigation, and intra-operative nerve monitoring, which greatly enhance safety. We can precisely remove problematic tissue (like a disc or bone spur) without harming surrounding nerves. Also, minimally invasive techniques mean smaller incisions, less muscle damage, and quicker recovery. As Dr. Murali Mohan notes, even complex spine deformity surgeries like scoliosis can now be corrected in a single stage without neurological complications, thanks to modern instrumentation and real-time monitoring. In fact, many spine surgeries that used to require long hospital stays are now done with early mobilization – some patients even go home within 24 hours for simpler procedures. Every surgery has some risks, but for a patient who truly needs it, spine surgery can be life-changing in a positive way – relieving pain, restoring mobility, and preventing long-term nerve damage. We always weigh the risks and benefits carefully. Remember, the goal is to improve your quality of life, not make it worse. With an experienced surgical team and proper patient selection, spine surgery today is very safe and often highly successful in doing just that.
A “slipped disc” refers to a disc prolapse or herniation, where one of the cushioning discs between your vertebrae bulges or ruptures and can press on nerves. Not all slipped discs require surgery – many improve with rest, physical therapy, or medications. However, if you have severe pain that doesn’t improve, significant leg pain (sciatica), numbness, or muscle weakness, or especially any bladder/bowel issues, then surgery might be the best option. The common surgery for this is a discectomy, where the herniated portion of the disc is removed to free the pinched nerve. This surgery is generally very safe and highly effective for relieving nerve pain. In fact, with modern techniques, a discectomy is often a minimal access or microsurgery done through a small incision. It can even be a day-care procedure now – patients often go home the same day and start walking immediately after surgery. The risk of complications like paralysis is extremely low (since we’re dealing with peripheral nerves, not the spinal cord in most lower back disc cases). Most patients notice a dramatic improvement in their leg or arm pain almost right after a successful disc surgery. So, if surgery is recommended because conservative measures failed, you can be reassured that it’s a routine, safe procedure with a high success rate.
This is an important discussion to have with the neurosurgeon. In general, if an aneurysm or AVM is considered high-risk for future rupture, treating it before it causes any harm is usually recommended. Factors like size, location, and your symptoms matter. For aneurysms, small ones (<5mm) in certain locations might be observed with serial scans, but larger ones or those with a concerning shape (bleb) often warrant treatment to preempt a bleed. For AVMs, doctors use a grading system to weigh the risk of surgery versus the risk of leaving it alone. Many unruptured AVMs, especially in younger patients, are treated electively because a successful treatment means you’re essentially cured and the lifelong risk of a brain bleed is gone. On the other hand, if an AVM or aneurysm is very small and in a very tricky location, sometimes monitoring might be advised – every case is unique. Rest assured, Dr. Murali Mohan S will carefully evaluate the specifics (for example, Is the aneurysm likely to rupture? Is the AVM in a part of the brain where treatment is very risky?) The decision is a balance of risks, but advances in treatment mean that if an aneurysm/AVM does need intervention, we have safe and effective ways to fix it. Many patients feel peace of mind after treatment, knowing they’ve been protected from a potential future hemorrhage. And indeed, outcomes are often excellent: treating a high-risk aneurysm early gives a patient a very good chance at a normal, healthy life without the worry of a rupture.
Treatment of an AVM is focused on preventing bleeding and improving the patient’s quality of life. There are a few options, and sometimes they are used in combination:
- Microsurgical Removal (Resection): If an AVM is in a favorable location, a neurosurgeon can perform an open brain surgery to carefully remove the tangle of vessels. This immediately eliminates the AVM. In fact, surgical removal is often the first choice for smaller AVMs or those causing symptoms, because once completely removed, the AVM is considered cured.
- Endovascular Embolization: This is a minimally invasive procedure where a catheter is navigated into the AVM and special glue-like substances or coils are injected to block blood flow into the tangle. Embolization can shrink the AVM or reduce blood flow, making subsequent surgery safer or occasionally obliterating the AVM if it’s small. It’s often used as a pre-surgical or pre-radiation adjunct, though in some cases, a series of embolizations can significantly reduce an AVM.
- Radiosurgery (Gamma Knife or similar): For smaller AVMs or those deep in the brain, a focused radiation treatment can be used. Highly focused beams of radiation cause the AVM vessels to scar and close off over time (typically 1–3 years). This is all done without any incision. Radiosurgery has a high success rate for appropriately sized AVMs, but it works gradually, and there is a risk the AVM could bleed in the meantime before it fully closes.
Often, a combination is employed – for example, an AVM might be embolized first to reduce its size, then surgically removed; or partially embolized and then treated with radiosurgery. The approach depends on the AVM’s size, location, and the patient’s overall condition. Dr. Murali and the team will discuss the best plan in your case. The ultimate goal is to completely eliminate the AVM or at least block it off so that it cannot bleed with as low risk as possible.
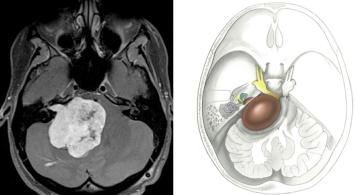
An AVM (Arteriovenous Malformation) is a tangle of abnormal blood vessels connecting arteries and veins in the brain (or spinal cord). It’s usually something people are born with (congenital), and over time it can cause trouble. An AVM creates a direct connection between arteries and veins, which can put a lot of pressure on those vessels. The biggest risk with an AVM is bleeding – if one of those vessels ruptures, it can cause a brain hemorrhage (bleed), similar to an aneurysm rupture. About half of brain AVMs are discovered only after they bleed. Besides bleeding, an AVM can also cause seizures, headaches, or neurological symptoms (like weakness or vision problems), because it can disrupt normal blood flow or press on brain tissue. Although AVMs are not cancer, they are serious because a rupture can lead to stroke, brain damage, or even death. The good news: AVMs can be treated to significantly reduce or eliminate these risks. Each AVM is unique in size and location, so treatment is individualized (it could be surgery, radiation, or other methods, as we’ll discuss next). Without treatment, there is a yearly risk of bleeding; with expert care, we aim to remove or obliterate the AVM and protect you from a potentially life-threatening hemorrhage
Not always – there are two main approaches to treat an aneurysm and prevent it from bleeding: microsurgical clipping and endovascular coiling. In clipping, a neurosurgeon performs a craniotomy (opens a small window in the skull) and places a tiny metal clip across the neck of the aneurysm. This clip seals off the aneurysm so blood can’t enter it, effectively eliminating the risk of rupture. Clipping has been used for decades and is very effective, with a low chance of the aneurysm ever coming back. The other approach is coiling, which is minimally invasive (no big opening in the skull). In coiling, a neuro-interventionist threads a catheter through an artery (usually from the groin or wrist) up into the brain and then fills the aneurysm with soft platinum coils or uses tiny flow-diverting stents. Coiling works by clotting off the inside of the aneurysm from within, so it can’t fill with blood. Both treatments have their pros and cons: clipping is a one-time durable fix (aneurysm rarely recurs), but involves open surgery, whereas coiling is less invasive with typically quicker recovery, but sometimes aneurysms can recur and need future check-ups. The choice depends on the aneurysm’s size, shape, location, and the patient’s overall health. Dr. Murali Mohan S and his team will evaluate what’s safest and best for your specific aneurysm. The goal in both methods is the same – to secure the aneurysm so it will not bleed.
A brain aneurysm is a weak, bulging spot on an artery in the brain, somewhat like a thin balloon. The danger is that an aneurysm can leak or rupture (burst open), causing bleeding in or around the brain – this is called a hemorrhagic stroke or subarachnoid hemorrhage, and it can be life-threatening. A ruptured aneurysm often causes a sudden, severe headache (“thunderclap headache”), loss of consciousness, or worse. Without treatment, a ruptured aneurysm can have devastating, life-changing consequences. The good news is that if we discover an aneurysm before it ruptures (for example, incidentally on a scan or due to warning symptoms), we can treat it to prevent a rupture. Even if it has ruptured, emergency treatment can save a life and often prevent further damage. In summary, a brain aneurysm is serious, but with early diagnosis and proper treatment, the chances of making a full recovery are quite good.
Recovery can vary, but many patients do remarkably well. After surgery, you will be monitored in the hospital for a few days. You might be surprised that mobilization (getting up and walking) is encouraged quite early – often within a day or two (or even the same day for many surgeries) under the guidance of the medical team. Pain from the incision or muscles can be managed with medication, and physical therapy will help you strengthen your back and limbs. If you had any weakness or numbness before surgery, those symptoms may gradually improve as the spinal cord or nerves recover from being compressed – nerves heal slowly, so it might take weeks to months for the full extent of improvement. In general, the prognosis is good if the tumor is removed successfully. Many patients are able to resume normal activities after a period of rehabilitation. For instance, in one case, a young army soldier presented with the tumour arising within the spinal cord in the cervical spine. We had operated him on 11th August; and he hoisted the flag on the occasion of Independence Day on 15th August. He joined his duties in 3 months time and is now completing his service. While each person’s case is unique, your surgical team will provide a tailored recovery plan. The key point is that, with modern techniques, spinal surgeries aim to not just remove the tumor but also help you return to a pain-free, functional life as quickly as possible.
Sometimes, yes. Certain spinal tumors involve not just the spinal cord but also the vertebrae (spinal bones) or the stability of the spine. If removing a tumor requires taking out part of a vertebra or destabilizes the spine, the surgeon will perform a spinal fusion in the same surgery to stabilize the area. This often involves placing screws and rods to support the spine’s structure. For example, tumors in the vertebral bone or surrounding the spinal cord can leave a gap or weaken the spine once removed – fusion bridges that gap and prevents any collapse or deformity. The need for fusion depends on the tumor’s location and size. Rest assured, if fusion is done, it’s to make sure you can move around safely after surgery without risking injury, and to allow the spine to heal in the correct alignment. Fusion facilitates patients to return to normal activities after recovery, in quick time.
Many spinal cord tumors can indeed be cured or effectively controlled by surgery, especially if they are benign. For example, tumors like schwannomas or meningiomas (common spinal tumors) are often benign and can be completely removed, which is curative. Even some intramedullary tumors (those inside the spinal cord), like certain ependymomas, can sometimes be fully resected and cured by surgery. If a tumor is malignant or metastatic, surgery can still be very beneficial: removing it relieves spinal cord pressure and pain, and it allows for other treatments (like radiation or chemotherapy) to work better on any remaining cancer. Each case is different – some small tumors that aren’t causing symptoms might be monitored rather than operated. But if a spinal tumor is operable and causing issues, surgery offers the best chance to alleviate symptoms and, in many cases, completely resolve the problem.
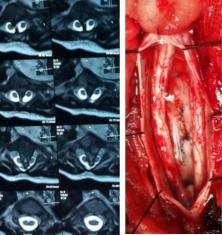
It’s natural to worry, but modern spinal tumor surgery is performed with very high precision to protect the nerves. Neurosurgeons use the operating microscope and delicate instruments to carefully dissect the tumor away from the spinal cord. We also employ intra-operative neuro-monitoring – this means we continuously check the function of spinal cord and nerves during the surgery (using electrical signals) to ensure we’re not harming them. Over the past few decades, there have been huge advances: in the 1980s and 90s, outcomes were more uncertain, but today’s technology (like high-powered drills for bone, microsurgical techniques, and constant nerve monitoring) makes these surgeries much safer. Removing the tumor often improves neurological function if the tumor was compressing the cord. The risk of serious complication like paralysis is quite low in experienced hands, and your surgical team will discuss specific risks based on your case. Overall, the goal is to remove the tumor completely (or as much as safely possible) while preserving and improving your nerve function.
A spinal cord tumor is an abnormal growth that develops either within the spinal cord or in the area around it (such as the coverings of the cord or the spine bones). Such a tumor can press on the spinal cord or nerves, leading to symptoms like back or neck pain, numbness or tingling in the limbs, weakness, or difficulty walking. Some spinal tumors are primary (originating in the spine) and often these are benign, like meningiomas or schwannomas. Others might be malignant or metastatic (spreading from cancers elsewhere). Regardless of type, if the tumor is causing neurologic symptoms or spinal instability, surgery is usually considered to remove it and relieve pressure on the spinal cord, which can prevent permanent nerve damage.
If the tumor is benign, surgery often cures it completely. After a successful removal of a benign tumor, no further treatment may be needed beyond routine follow-up scans. If the tumor is malignant or very aggressive, surgery is usually the first step – it will relieve symptoms and reduce tumor size, but additional treatments (like radiation or chemotherapy) may be recommended afterward to target any remaining tumor cells. As for recovery, it varies with the complexity of surgery and the patient’s condition. Many patients are awake and talking later the same day of surgery or by the next day. You might spend a couple of days in the ICU or hospital for monitoring. In patients who present late with neurological issues, thanks to refined techniques, rehabilitation is much faster now – most people can start gentle activities within days. The full recovery can take a few weeks to a few months, but patients often return to their normal routines much sooner than they expect, especially with the support of physiotherapy and modern post-operative care. Importantly, if surgery is done before significant brain damage occurs, many patients experience a big improvement in symptoms (like headaches or seizures) after the tumor is removed.
Neurosurgeons take great care to protect normal brain tissue. First, detailed imaging (MRI, etc.) helps us plan a safe path to the tumor. During surgery, we often use a powerful operating microscope for magnification, giving a very clear view of tiny structures. We also utilize neuro-monitoring – attaching electrodes to monitor brain and nerve function in real time – so if we get too close to critical areas, we know immediately. For tumors located in or near vital regions (like areas controlling speech or movement), we might employ an awake surgery technique as mentioned, where the patient can respond to tasks during the operation. This way, we map out essential brain functions and remove the tumor without causing neurological deficits. By combining these strategies, surgeons are able to maximize tumor removal and minimize risks of injury to the brain.
Yes, modern brain tumor surgery is much safer than in the past, thanks to advanced technology and techniques. We now use high-resolution MRI scans and sometimes CT scans to map the tumor before surgery, and during the operation we have tools like intraoperative ultrasound and neuro-monitoring and high precision Neuro Navigation to guide us. Advanced Microscopes and Instruments such as CUSA helps the surgeon deal with difficult scenarios. These advances help surgeons achieve near-total removal of tumors while protecting healthy brain tissue. In some cases, we perform “awake craniotomy” for tumors near critical brain areas – the patient is kept comfortable and pain-free, but awake enough to follow commands, so we can test their speech or movements during surgery. This technique allows precise mapping of important functions and helps avoid any damage while removing the tumor. Overall, outcomes have improved dramatically – patients tolerate brain surgery better and recover faster today than a few decades ago.
No, not all brain tumors are cancerous. Many brain tumors (for example, meningiomas) are benign, meaning they do not spread to other parts of the body. But even benign brain tumors can cause symptoms (headaches, seizures, memory or vision changes, etc.) by compressing brain structures, so they shouldn’t be ignore. The good news is that benign tumors are often curable with surgery alone. Malignant (cancerous) brain tumors may require a combination of treatments – surgery to remove as much tumor as safely possible, followed by chemotherapy or radiation. The surgical approach is determined by the tumor’s location, type, and size. Your neurosurgeon will tailor the treatment to whether the tumor is benign or malignant, always aiming to maximize tumor removal while preserving your quality of life.
A brain tumor is an abnormal growth of cells in the brain. Not all brain tumors are cancerous (malignant); many are benign (non-cancerous). However, even benign tumors can cause serious problems by pressing on normal brain tissue, so they often require treatment. Surgery is usually the first line of treatment for accessible brain tumors because removing the tumor relieves pressure on the brain. In benign tumors, surgical removal can even result in a complete cure. For malignant tumors, surgery helps by reducing the tumor’s size (tumor “burden”), which makes follow-up treatments like radiation or chemotherapy more effective. In short, surgery helps preserve brain function and can significantly improve symptoms.
Avoid sudden movements, bending, or twisting your spine. Use proper techniques to get out of bed, and follow strictly the advice regarding walking and wearing a brace as recommended.
Lifting should be limited to light objects, typically no more than 5 kilograms, during the initial recovery phase. Gradually increase lifting capacity as advised during follow-ups, based on your progress and strength. Its essential to gradually build the core strength along with regular exercises to increase the weight lifting capacity.
While spine surgery can effectively alleviate pain and improve mobility, the overall success often depends on post-operative care and lifestyle changes. Adhering to the advice concerning do's and dont's, engaging in recommended exercises, and maintaining a healthy lifestyle are key to achieving long-term results.
Maintaining a healthy weight, practicing good posture, avoiding smoking, and staying active with doctor-recommended exercises are essential for preventing future spine issues. Additionally, regular follow-ups and listening to your body can help address concerns early and maintain spine health.
Mild discomfort or pain is normal during the recovery period and typically improves over time. However, persistent, severe, or worsening pain should be promptly reported for further evaluation.
In the long term, most patients can resume normal activities without major restrictions. However, it's advised to avoid heavy lifting, high-impact activities, and prolonged sitting for extended periods, especially during the first few months. Regular exercises and maintaining proper posture can help prevent future issues.
The timeline for returning to work depends on the nature of your job. For desk jobs or roles involving minimal physical activity, most patients can resume work within 1–2 weeks. For physically demanding jobs, the recovery period may be longer, and it's essential to follow the advice during follow-up consultations.
Most patients are mobilized the same day after surgery, which significantly reduces the need for prolonged physical therapy. However, specific exercises or therapy are crucial to ensure optimal recovery. Spinal surgeries correct structural issues, but rebuilding muscular strength remains essential, emphasising the importance of tailored physical therapy and consistent exercise.
Light activities can typically be resumed within a days, with most patients returning to their routine within two weeks. Strenuous activities, however, should only be undertaken after first consultation after the surgery.
Recovery varies, but most patients start feeling better the same day in the evening and are encouraged to walk. Those who don’t walk the same day are ensured that they walk the next day! With such quick recovery, the confidence builds up and they can get back to their routine life in a maximum of 2 weeks.
https://maps.app.goo.gl/CgH98dCkUPf1b3sA6
https://maps.app.goo.gl/yoQctYsXkDqb2j2FA
The In-patient admissions and surgical services of Dr Murali are available at Sparsh Hospitals, Hennur, Bengaluru, India.
The International / Foreign nationals can reach out @ +91 9900701080 by Whatsapp or Call, to schedule an appointment.
The may share the previous records and available reports with summary - for an online opinion.
Yes, you may reach out with your request for rescheduling at your nearest convenient location ( Yelahanka / Jayanagar / Yeshwanthpur) by contacting us on +91 9900701080 / 9686911560
If you had booked the Appointment through the Smart Appointments on the Dashboard, you can cancel and rebook the appointment, all by yourself ; or reach out for help at the given numbers- above
Dr Murali doesn't consult online. However, You can reach out with reports and detail on Whatsapp for a free opinion @ +91 9900701080
For Appointment at Sparsh Hospitals, Hennur; You can avail the option of 'Appointment Request', on LinQMD profile page of Dr Murali. Once the appointment is booked, you will get the Confirmation of Appointment from the Doctor's office.
For Appointments at Synapse Clinics at Yelahanka and Jayanagar, Please directly book the appointments through the Dashboard; Alternatively you may call up: 9900701080 / 9686911560
Definitely yes, You can avail the facility. However the extent of coverage depends upon your policy terms with the policy provider.
You may reach out to our coordinator on +91 9900701080 / 9686911560 with your policy details to ascertain your Insurance coverage.